Mucocele Treatment: Symptoms, Causes & Home Remedies Guide
Discover effective home remedies and medical treatments for mucocele relief
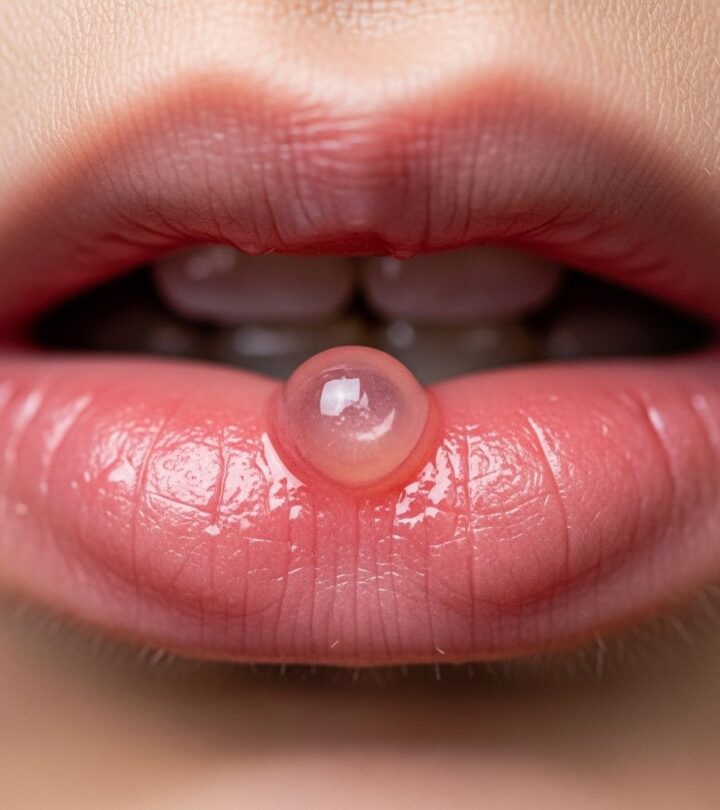
Image: ShutterStock
A mucocele is a harmless, fluid-filled cyst that commonly appears on the inside of the lips, cheeks, or other areas of the mouth. These small, dome-shaped bumps develop when salivary glands become blocked or damaged, causing mucus to accumulate beneath the surface of the oral tissue. While mucoceles are typically painless and benign, they can cause discomfort and concern for those experiencing them. Understanding the causes, symptoms, and available treatment options—including effective home remedies—can help you manage this common oral condition effectively.
What Is a Mucocele?
A mucocele, also known as a mucous cyst or oral mucous cyst, is a clear or bluish bump that forms when a salivary gland duct becomes blocked or damaged. The term comes from the Latin words “mucus” (slime) and “cele” (cavity). These cysts occur when saliva cannot drain properly from the minor salivary glands, leading to fluid accumulation in the surrounding soft tissue. Mucoceles are among the most common oral lesions, accounting for approximately 5.6% of all oral biopsies.
The lower lip is the most frequent location for mucoceles, representing about 88% of cases. However, they can also appear on the buccal mucosa (inside the cheeks), the floor of the mouth, the tongue, and occasionally the palate. When a mucocele occurs on the floor of the mouth, it is specifically called a ranula, which can sometimes grow larger and potentially affect breathing in rare cases.
Most mucoceles are classified into two types based on their formation mechanism. Extravasation mucoceles are the most common type, resulting from trauma that ruptures a salivary duct, causing mucus to spill into surrounding tissues. Retention mucoceles form when a salivary duct becomes blocked, causing mucus to back up within the gland itself. Despite these different mechanisms, both types present similarly and are managed using the same treatment approaches.
Recognizing Mucocele Symptoms
Identifying a mucocele is relatively straightforward due to its characteristic appearance and presentation. The typical mucocele appears as a soft, round, dome-shaped swelling that ranges from a few millimeters to over a centimeter in diameter. The overlying tissue often has a translucent, bluish, or clear appearance, allowing the fluid content to show through the thin membrane.
Most mucoceles are completely painless, though larger ones may cause mild discomfort, especially when eating, speaking, or brushing teeth. The cyst has a fluctuant quality, meaning it feels soft and fluid-filled when gently pressed. Some patients report that their mucocele periodically ruptures, releasing a clear, sticky, mucous-like fluid before reforming again.
Key symptoms and characteristics include:
Appearance: Smooth, round bump with a bluish or translucent surface that clearly distinguishes it from other oral lesions.
Location: Most commonly on the inner lower lip, but can occur on the cheeks, tongue, floor of mouth, or palate.
Size variation: Can range from very small (2-3mm) to quite large (over 1cm), with size sometimes fluctuating as the cyst fills and drains.
Pain level: Generally painless, though may cause discomfort if large enough to interfere with normal oral functions.
Recurrence: May spontaneously rupture and reform multiple times, creating a cycle of disappearance and reappearance.
While mucoceles are typically benign, it’s important not to self-diagnose oral lesions. Any persistent bump or growth in the mouth should be evaluated by a healthcare professional to rule out more serious conditions, including oral cancer.
Common Causes of Mucocele Formation
Understanding what causes mucoceles can help in both treatment and prevention. The primary cause of mucocele formation is trauma to the oral tissues that damages the minor salivary glands or their ducts. This trauma can be acute (a single injury) or chronic (repeated minor injuries over time).
The pathogenesis involves traumatic rupture of a mucous duct, leading to the outpouring of sialomucin (the protein-rich mucus produced by salivary glands) into the surrounding connective tissue. When mucus escapes from the duct system, the body recognizes it as a foreign substance and walls it off, creating the characteristic cyst.
Common traumatic causes include:
Habitual lip or cheek biting: This is perhaps the most common cause, often occurring unconsciously during stress, anxiety, or concentration.
Accidental trauma: Biting the inside of your mouth while eating or talking can damage salivary ducts.
Dental procedures: Oral surgery, dental injections, or aggressive dental work can occasionally traumatize minor salivary glands.
Piercings: Oral piercings can damage salivary tissue and lead to mucocele formation.
Poor-fitting dental appliances: Dentures, braces, or retainers that rub against oral tissues can cause repeated trauma.
Sports injuries: Impact to the mouth during athletic activities can damage salivary structures.
Certain behaviors and conditions may increase mucocele risk. Chronic lip biting, often associated with anxiety or stress, creates repeated microtrauma to the delicate salivary ducts. Smoking contributes to oral tissue irritation and may slow healing, potentially increasing mucocele susceptibility. Additionally, individuals who engage in contact sports without protective mouthguards face higher risk of oral trauma that can lead to mucocele development.
Effective Home Remedies for Mucocele
For minor mucoceles, several home remedies can help reduce inflammation, support healing, and provide relief while the body naturally resolves the cyst. While these remedies may not eliminate large or persistent mucoceles, they can be effective for smaller lesions and provide symptomatic relief.
Saltwater Rinses
Warm saltwater rinses are one of the most effective and accessible home treatments for mucoceles. Salt water creates a hypertonic environment that can help reduce inflammation, draw out excess fluid, and promote healing. To prepare a saltwater rinse, dissolve one teaspoon of salt in a cup of warm (not hot) water. Swish the solution gently in your mouth for 30 seconds to one minute, focusing on the affected area, then spit it out. Repeat this process several times daily, especially after meals and before bed.
The antimicrobial properties of salt also help prevent secondary infection, which is important for optimal healing. This simple remedy supports the body’s natural healing process and can accelerate the resolution of smaller mucoceles.
Honey Application
Raw honey has been used for centuries as a natural healing agent, and research supports its antimicrobial and anti-inflammatory benefits. Honey can help reduce infection risk and promote tissue healing when applied directly to a mucocele. Choose raw, organic honey for maximum therapeutic benefit, as processed honey may lack the beneficial enzymes and compounds found in its natural form.
To use honey for mucocele treatment, apply a small amount directly to the cyst using a clean finger or cotton swab. Leave it in place for 10-15 minutes before rinsing with warm water. Repeat this application two to three times daily. The natural antibacterial properties of honey help keep the area clean while supporting the healing process.
Aloe Vera Gel
Aloe vera gel offers soothing and anti-inflammatory properties that can benefit mucocele management. Preliminary research suggests that aloe vera’s bioactive compounds may support healing of oral lesions, though more clinical studies are needed to fully establish its efficacy. Apply pure aloe vera gel directly to the mucocele to reduce irritation and promote healing.
Use fresh aloe vera gel extracted from the plant or a high-quality, pure commercial product without added chemicals or alcohol. Apply the gel gently to the affected area and leave it in place for 15-20 minutes before rinsing. You can repeat this application several times daily for best results.
Ice Compress
Applying cold compresses can help reduce swelling and numb any discomfort associated with larger mucoceles. Wrap ice cubes in a clean cloth or use a cold compress and apply it to the outside of your lip or cheek near the mucocele for 10-15 minutes at a time. This can be particularly helpful if the mucocele is causing tenderness or interfering with eating or speaking.
Turmeric Paste
Turmeric contains curcumin, a compound with powerful anti-inflammatory and antimicrobial properties. Create a paste by mixing turmeric powder with a small amount of water or honey, and apply it directly to the mucocele. Leave the paste in place for 10-15 minutes before rinsing thoroughly. Be aware that turmeric can temporarily stain tissues yellow, but this discoloration is harmless and will fade.
Important Precautions with Home Remedies
While natural remedies can provide relief, they are generally less effective than medical treatments for persistent or large mucoceles. Never attempt to rupture, puncture, or remove a mucocele yourself, as this can lead to infection, scarring, or recurrence. Home remedies work best for minor mucoceles and should be used as complementary approaches alongside professional medical care when needed.
Monitor the mucocele regularly to ensure it is not growing, becoming infected, or causing increasing discomfort. If home treatment doesn’t show improvement within two weeks, or if the mucocele worsens, seek professional evaluation.
Medical Treatment Options for Mucocele
When home remedies prove insufficient or when dealing with larger, persistent, or recurrent mucoceles, medical intervention becomes necessary. Healthcare providers offer several treatment approaches depending on the mucocele’s size, location, and individual patient factors.
Corticosteroid Injections
For recurrent or persistent mucoceles that don’t respond to home care, intralesional corticosteroid injections offer a non-invasive treatment option. This approach involves injecting a corticosteroid medication directly into the mucocele to reduce inflammation and shrink the cyst. Case studies suggest this method may be particularly beneficial for children, providing a safer alternative to surgery while minimizing risks such as duct damage and recurrence.
The procedure is relatively quick and can be performed in an office setting. Multiple injections may be necessary for complete resolution, but this approach avoids the risks associated with surgical procedures.
Sclerotherapy
Sclerotherapy involves injecting a sclerosing agent into the mucocele to cause the cyst to shrink and eventually disappear. Sodium tetradecyl sulfate (STS) and polidocanol are commonly used sclerosants for this purpose. This treatment works by irritating the cyst lining, causing it to collapse and seal shut.
A case report documented complete resolution of a mucocele on the buccal mucosa after two sessions of sclerotherapy with STS, with no recurrence after six months. Another case showed complete disappearance of a lower lip mucocele within three weeks of STS treatment. This approach is particularly useful for mucoceles in locations that are difficult to access surgically, such as the posterior buccal mucosa.
Surgical Excision
Surgical removal remains the most common and definitive treatment for mucoceles, especially for large or frequently recurring cysts. The procedure typically involves complete excision of the mucocele along with the associated damaged salivary gland to prevent recurrence. Surgery is usually performed under local anesthesia as an outpatient procedure.
The surgeon removes not only the cyst but also the adjacent minor salivary glands to eliminate the source of mucus production that led to the mucocele formation. This comprehensive approach significantly reduces the likelihood of recurrence compared to simple drainage or partial removal.
Laser Surgery
Laser treatment offers a modern alternative to traditional surgical excision, using targeted light energy to remove the mucocele with minimal bleeding and quicker recovery. CO2 lasers and diode lasers are commonly used for this purpose. The laser simultaneously cuts and cauterizes tissue, reducing bleeding and potentially decreasing post-operative discomfort.
Benefits of laser surgery include reduced operative time, less post-operative swelling, minimal scarring, and faster healing compared to conventional surgery. However, this option may not be suitable for all mucoceles, particularly very deep or large lesions.
Post-Treatment Care
Regardless of the treatment method chosen, proper post-operative care is essential for optimal healing and preventing recurrence. Follow your healthcare provider’s instructions carefully, which typically include maintaining excellent oral hygiene, avoiding trauma to the treated area, and attending all follow-up appointments to monitor healing.
Prevention Strategies for Mucocele
Preventing mucoceles centers on avoiding oral trauma and maintaining excellent oral health. Since most mucoceles result from injury to salivary glands or ducts, reducing traumatic incidents significantly lowers your risk of developing these cysts.
Breaking Harmful Habits
The most important preventive measure is to stop habitual lip or cheek biting. This unconscious behavior, often triggered by stress, anxiety, or boredom, is the leading cause of mucocele formation. To break this habit, start by identifying your triggers—keep a journal to note when and why you bite your lips or cheeks. Once you recognize the patterns, you can develop strategies to address them.
Substituting the behavior with a healthier alternative can help. Chewing sugar-free gum provides oral stimulation without causing tissue damage. Stress-reduction techniques such as deep breathing, meditation, or regular exercise can address the underlying anxiety that often drives these habits. Some people find that applying lip balm frequently makes them more conscious of their lips and helps interrupt the biting behavior.
Maintaining Oral Hygiene
Good oral hygiene helps prevent infections that could trigger or complicate mucoceles. Brush your teeth at least twice daily with a soft-bristled toothbrush, and floss regularly to remove food particles and bacteria. Use gentle, circular motions when brushing to avoid traumatizing oral tissues. Consider using an antimicrobial mouthwash to further reduce bacterial load in your mouth.
Using Protective Equipment
For individuals who participate in contact sports or activities with risk of oral injury, wearing a properly fitted mouthguard is essential. Custom-fitted mouthguards provided by your dentist offer the best protection, though over-the-counter options are also available. If you grind or clench your teeth at night (bruxism), a night guard can protect your oral tissues from trauma during sleep.
Addressing Dental Appliances
Ensure that dentures, braces, retainers, or other dental appliances fit properly and aren’t rubbing against your oral tissues. Poor-fitting appliances can cause chronic irritation that damages salivary glands. If you notice any sharp edges or areas of discomfort, contact your dentist for adjustments.
Lifestyle Modifications
Quitting smoking supports overall oral health and may reduce mucocele risk. Smoking irritates oral tissues and impairs healing, potentially making you more susceptible to various oral conditions including mucoceles. Additionally, be mindful when eating—chewing slowly and carefully reduces the risk of accidentally biting your cheeks or lips.
Regular Dental Visits
Schedule routine dental checkups every six months to enable early detection of mucoceles or other oral issues. Your dentist can identify potential problems before they become symptomatic and provide guidance on preventing oral trauma. Professional cleanings also support overall oral health, creating an environment less conducive to complications.
When to Seek Professional Medical Care
While many small mucoceles resolve on their own or with home treatment, certain situations warrant professional evaluation and care. Recognizing when to consult a healthcare provider ensures proper diagnosis and treatment, preventing potential complications.
Seek medical attention if:
The mucocele persists for more than two weeks despite home treatment.
The cyst is growing larger or changing in appearance.
You experience increasing pain, tenderness, or discomfort.
Signs of infection develop, such as redness, warmth, pus, or fever.
The mucocele interferes with eating, speaking, or swallowing.
You have recurrent mucoceles that repeatedly form in the same location.
The lesion is located on the floor of your mouth (ranula), especially if it’s large.
You’re uncertain whether the bump is actually a mucocele or could be something else.
A healthcare provider can accurately diagnose the condition through physical examination and, if necessary, biopsy to rule out other oral lesions. Early intervention can prevent complications and ensure you receive the most appropriate treatment for your specific situation.
Understanding the Prognosis and Outlook
The prognosis for oral mucoceles is generally excellent. Most mucoceles are painless, superficial cysts that do not cause long-term complications. Small mucoceles often resolve spontaneously without any treatment, while others respond well to conservative home remedies or medical interventions.
After proper treatment, whether through home care, medical management, or surgery, most people experience complete resolution with no lasting effects. However, mucoceles can recur, particularly if the underlying cause (such as habitual lip biting) is not addressed. Recurrence rates vary depending on the treatment method used, with complete surgical excision of the affected gland offering the lowest recurrence rates.
Larger mucoceles may interfere with normal oral functions such as speaking, chewing, and swallowing if left untreated. Ranulas, which form on the floor of the mouth, can occasionally grow large enough to cause breathing difficulties, though this is rare. These potential complications underscore the importance of monitoring mucoceles and seeking treatment when they persist or cause problems.
With appropriate treatment and preventive measures, most individuals can eliminate mucoceles and prevent future occurrences. The key is addressing both the lesion itself and any contributing factors, such as oral habits or dental issues, that may have caused it in the first place.
Frequently Asked Questions About Mucocele
Can I pop or drain a mucocele myself?
No, you should never attempt to pop, puncture, or drain a mucocele yourself. Doing so can introduce bacteria leading to infection, cause scarring, damage surrounding tissues, and often leads to recurrence. Always seek professional treatment for mucocele removal.
How long does it take for a mucocele to go away on its own?
Small mucoceles may resolve spontaneously within a few weeks, though some persist for months. The healing timeline varies based on size, location, and whether the underlying cause continues. If a mucocele doesn’t improve within two weeks of home treatment, consult a healthcare provider.
Are mucoceles contagious?
No, mucoceles are not contagious. They result from trauma to salivary glands and cannot be transmitted from person to person through contact or any other means.
Can mucoceles turn into cancer?
Mucoceles are benign lesions and do not become cancerous. However, any persistent oral lesion should be evaluated by a healthcare professional to ensure accurate diagnosis and rule out other conditions, including oral cancer.
Will a mucocele come back after treatment?
Recurrence is possible, especially if the underlying cause isn’t addressed. Surgical excision that removes the affected salivary gland has the lowest recurrence rate. Preventing habits like lip biting significantly reduces the likelihood of new mucocele formation.
Is surgical removal of a mucocele painful?
The procedure itself is performed under local anesthesia, so you shouldn’t feel pain during surgery. Some discomfort or soreness is normal during the healing period, but this can typically be managed with over-the-counter pain medications as recommended by your healthcare provider.
Can children get mucoceles?
Yes, children can develop mucoceles, often from accidental trauma or lip biting. Pediatric mucoceles are typically managed similarly to those in adults, though less invasive options like corticosteroid injections may be preferred initially to avoid surgical intervention in young patients.
What’s the difference between a mucocele and a canker sore?
Mucoceles are fluid-filled cysts that appear as clear or bluish bumps, while canker sores are painful ulcers with a white or yellow center surrounded by red inflammation. Canker sores are open lesions, whereas mucoceles are raised, fluid-filled bumps beneath intact mucosa.
Key Takeaways
Mucoceles are common, benign oral cysts caused by blocked or damaged salivary glands, most frequently resulting from trauma to the oral tissues. While these clear or bluish bumps typically appear on the lower lip, they can occur anywhere in the mouth where minor salivary glands exist. Most mucoceles are painless and may resolve spontaneously, though larger or persistent lesions often require intervention.
Home remedies including saltwater rinses, honey applications, and aloe vera gel can effectively manage minor mucoceles by reducing inflammation and supporting natural healing processes. These conservative approaches work best for small lesions and should be attempted before considering more invasive treatments. However, natural remedies are generally less effective than medical treatments for persistent or large mucoceles.
Medical interventions range from non-invasive options like corticosteroid injections and sclerotherapy to definitive surgical removal. The choice of treatment depends on factors including mucocele size, location, duration, and individual patient circumstances. Surgical excision remains the gold standard for preventing recurrence, particularly when combined with removal of the affected salivary gland.
Prevention focuses on avoiding oral trauma by breaking habits like lip or cheek biting, maintaining excellent oral hygiene, using protective mouthguards during sports, and ensuring dental appliances fit properly. Quitting smoking and addressing stress that triggers harmful oral habits also contribute to prevention efforts.
If you suspect you have a mucocele, consult your dentist or healthcare provider for accurate diagnosis and appropriate treatment recommendations. While many mucoceles are harmless and self-limiting, professional evaluation ensures you’re not dealing with a more serious condition and provides access to effective treatment options when needed. Early intervention and addressing underlying causes offer the best outcomes for both treatment and prevention of these common oral lesions.
References
- https://www.rupahealth.com/post/oral-mucocele-symptoms-causes-treatment-and-prevention
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9855259/
- https://www.trysnow.com/blogs/news/clear-bump-inside-lip
- https://www.stylecraze.com/articles/home-remedies-to-treat-mucocele/
- https://www.news-medical.net/health/Mucocele-Treatment.aspx
- https://jamanetwork.com/journals/jamadermatology/fullarticle/531639
- https://www.colgate.com/en-us/oral-health/mouth-sores-and-infections/mucoceles-and-how-to-treat-them
- https://amj.amegroups.org/article/view/9306/html
- https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/602892
Read full bio of Medha Deb