Anal Fissure Treatment: Complete Guide to Healing & Relief
Discover effective anal fissure treatments, from home remedies to medical interventions for lasting relief
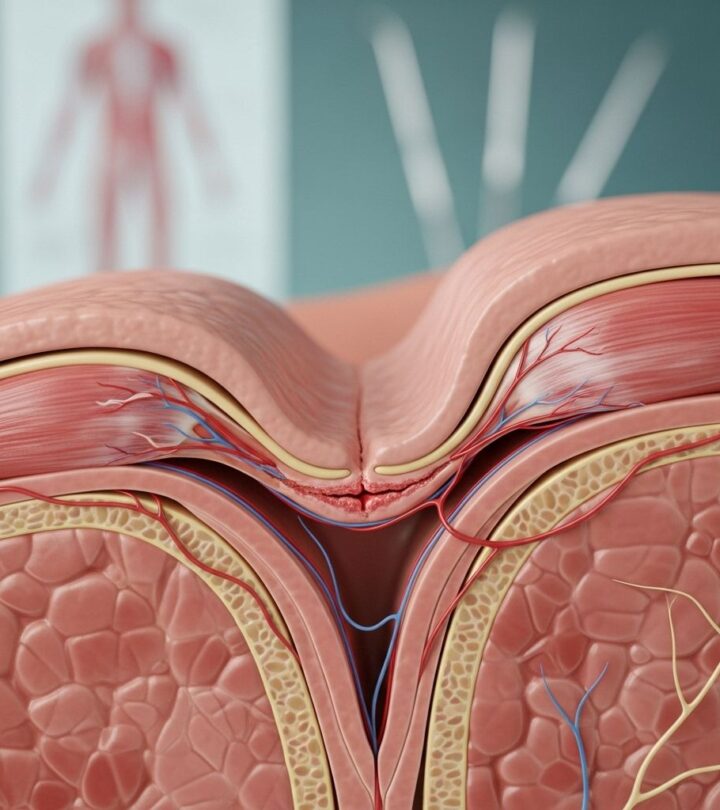
Image: ShutterStock
An anal fissure is a painful tear or split in the delicate lining of the anus that can cause significant discomfort during and after bowel movements. This common condition affects people of all ages and can range from acute cases that heal quickly to chronic fissures that persist for weeks or months. Understanding the various treatment options available is essential for anyone experiencing this uncomfortable condition, as proper treatment can dramatically improve quality of life and promote faster healing.
The pain associated with anal fissures occurs due to a cycle of trauma and muscle spasm. When the sensitive tissue tears, it triggers intense pain that causes the anal sphincter muscle to contract involuntarily. This spasm reduces blood flow to the area, which slows the healing process and makes future bowel movements even more painful, potentially causing further tearing. Breaking this cycle requires a comprehensive treatment approach that addresses both the immediate symptoms and the underlying causes.
Understanding Anal Fissure Development
Before exploring treatment options, it’s important to understand how anal fissures develop and what factors contribute to their formation. The most common cause of anal fissures is trauma from passing hard or large stools during constipation. The stretching of the anal canal beyond its capacity creates small tears in the sensitive mucosal lining. However, other factors can also contribute to fissure development, including chronic diarrhea, inflammatory bowel diseases, reduced blood flow to the anorectal area, and childbirth.
Anal fissures are classified as either acute or chronic based on their duration and characteristics. Acute fissures are fresh tears that typically appear as clean cuts and can heal within a few weeks with appropriate treatment. Chronic fissures, on the other hand, persist for more than eight weeks and often develop additional features such as a skin tag at the external end or exposed muscle fibers at the base. Chronic fissures are more challenging to treat and may require more intensive interventions beyond simple home remedies.
Conservative Home Treatment Approaches
The foundation of anal fissure treatment begins with conservative home care measures that can effectively heal many acute fissures without the need for medical intervention. These approaches focus on reducing trauma to the affected area, promoting softer bowel movements, and creating optimal conditions for natural healing. Most healthcare professionals recommend starting with these conservative measures, as nearly half of all acute anal fissures will resolve with nonoperative treatment alone.
Dietary modifications form the cornerstone of home treatment for anal fissures. Increasing fiber intake is crucial for softening stools and reducing strain during bowel movements. A high-fiber diet should include plenty of fresh fruits, vegetables, and whole grains. The goal is to achieve one soft, well-formed bowel movement per day, which minimizes trauma to the healing fissure. Patients should aim for 25-35 grams of fiber daily through food sources or supplements.
Adequate hydration works synergistically with increased fiber intake to maintain soft stools. Drinking at least eight 8-ounce glasses of non-caffeinated, non-alcoholic fluids daily helps prevent constipation and reduces the likelihood of hard stools that can reinjure the fissure. Water remains the best choice for hydration, though herbal teas and clear soups can also contribute to fluid intake goals.
Fiber Supplements and Stool Softeners
When dietary changes alone are insufficient to achieve soft, regular bowel movements, fiber supplements and stool softeners become valuable additions to the treatment regimen. These products help maintain stool consistency and reduce the mechanical trauma that can prevent fissure healing or cause recurrence.
Bulk-forming laxatives such as psyllium (Metamucil), methylcellulose (Citrucel), or calcium polycarbophil (Fibercon) add bulk and water to stools, making them softer and easier to pass. These supplements should be taken consistently, typically one tablespoon in liquid form or two capsules three times daily with meals. It’s essential to take these supplements with adequate water to prevent them from causing intestinal obstruction.
Stool softeners like docusate sodium (Colace) work by allowing water and fats to penetrate the stool, making it softer and easier to pass. A typical dosage is 100mg taken three times daily with meals. Unlike stimulant laxatives, stool softeners don’t cause dependency and can be used long-term to maintain soft stools and prevent fissure recurrence.
The Therapeutic Benefits of Sitz Baths
Sitz baths represent one of the most effective and soothing home treatments for anal fissures. This simple therapy involves sitting in warm water that covers only the hips and buttocks, providing multiple therapeutic benefits that promote healing and pain relief. The warm water helps relax the anal sphincter muscle, reducing spasm and improving blood flow to the affected area. This increased circulation delivers more oxygen and nutrients to the fissure, accelerating the healing process.
For optimal results, patients should soak in 8 to 10 centimeters of warm water for 10 to 20 minutes several times throughout the day, especially after each bowel movement. The water should be comfortably warm but not hot enough to cause burns. Adding Epsom salts to the water may provide additional relief, though plain warm water is equally effective. Regular sitz baths can significantly reduce pain and discomfort while creating an environment conducive to healing.
Perianal Skin Care and Hygiene
Proper perianal hygiene is essential for preventing infection and promoting healing of anal fissures. The delicate skin around the anus requires gentle care to avoid further irritation or damage. Harsh cleaning methods or irritating products can exacerbate pain and delay healing, making thoughtful hygiene practices an important component of fissure management.
After bowel movements, patients should use pre-moistened wipes that do not contain witch hazel or alcohol, as these ingredients can cause stinging and irritation. Baby wipes or Cottonelle wipes are good choices for gentle cleansing. Products containing witch hazel, such as Tucks pads or Preparation H wipes, should be avoided despite their popularity for hemorrhoid treatment. Regular soap should not be applied directly to the perianal skin, as it can strip away natural oils and cause dryness and irritation.
Patients should pat the area dry gently rather than rubbing vigorously. Wearing loose, breathable cotton underwear allows air circulation and prevents moisture accumulation, which can promote bacterial growth and delay healing. Some individuals find that briefly air-drying the area after cleaning and before dressing provides additional comfort and promotes healing.
Topical Medications for Sphincter Relaxation
When conservative measures prove insufficient, topical medications that relax the anal sphincter muscle become the next line of treatment. These medications work by reducing the excessive muscle tone that characterizes anal fissures, thereby improving blood flow to the area and breaking the pain-spasm cycle that prevents healing. Several topical agents have proven effective for treating anal fissures, each with distinct mechanisms of action and side effect profiles.
Topical nitroglycerin is generally considered the first-choice medical treatment when conservative measures fail. Available as Rectiv or compounded in concentrations of 0.2% to 0.4%, nitroglycerin acts as a vasodilator that increases blood flow to the fissure while relaxing the internal anal sphincter. Patients typically apply a small amount to the perianal skin outside the anus twice daily. The medication promotes healing and reduces pain, though headaches represent a common and sometimes severe side effect. Patients should apply nitroglycerin while seated and avoid standing too quickly to prevent dizziness. Additionally, medications such as sildenafil, tadalafil, and vardenafil should be avoided during nitroglycerin treatment due to potentially dangerous interactions.
Topical calcium channel blockers, specifically nifedipine (0.2%-0.5%) and diltiazem (2%), offer alternatives to nitroglycerin with potentially fewer side effects. These medications relax the anal sphincter by reducing muscle tone, which promotes blood flow and faster healing. Diltiazem cream is typically applied as a marble-sized amount (approximately ½ inch) to the perianal skin twice daily. Studies have demonstrated that topical nifedipine achieves higher healing rates compared to nitroglycerin while causing fewer side effects, particularly headaches. If the cream is wiped off after a bowel movement, patients should reapply it to maintain therapeutic levels.
Topical anesthetic creams containing lidocaine (2% lidocaine jelly or Xylocaine) provide temporary pain relief, making bowel movements more tolerable. While these creams don’t directly promote healing, they help break the fear-pain cycle that can lead to voluntary stool retention and worsening constipation. Compounded combinations of topical nifedipine and lidocaine may provide both pain relief and sphincter relaxation in a single application.
Injectable Botulinum Toxin Treatment
Botulinum toxin type A, commonly known as Botox, represents an intermediate treatment option between topical medications and surgery for patients with chronic anal fissures that haven’t responded to conservative treatments. This injection therapy temporarily paralyzes the internal anal sphincter muscle, reducing spasms and allowing the fissure to heal without the permanence of surgical intervention.
Botox works by blocking nerve signals that cause muscle contractions. When injected into the internal anal sphincter, it reduces muscle pressure and tension, which improves blood flow to the fissure and creates conditions favorable for healing. The procedure is performed in a medical office or outpatient setting and typically takes only a few minutes. The effects of Botox injections last approximately three to four months, during which time the fissure has an opportunity to heal completely.
This treatment option offers several advantages over surgery, including lower risk of permanent incontinence and the reversible nature of the muscle relaxation. However, multiple injections may be necessary if the fissure doesn’t heal during the initial treatment period. Success rates for Botox injections range from 60% to 80%, making them less effective than surgery but more effective than topical treatments alone for chronic fissures.
Surgical Treatment Options
When chronic anal fissures resist conservative treatments, medications, and injectable therapies, surgical intervention may become necessary. Surgery is typically reserved for fissures that have persisted for more than eight weeks despite appropriate medical management, or for cases causing severe symptoms that significantly impact quality of life. The surgical approach offers the highest success rates for chronic fissures but also carries small risks that must be carefully considered.
Lateral Internal Sphincterotomy (LIS) represents the gold standard surgical procedure for chronic anal fissures. This operation involves cutting a small portion of the internal anal sphincter muscle to permanently reduce tension and improve blood flow to the area. The procedure can be performed under local anesthesia with sedation or general anesthesia, and most patients can return home the same day.
During LIS, the surgeon makes a small incision and carefully divides a portion of the internal sphincter muscle. This controlled weakening of the muscle permanently reduces the excessive pressure that prevents fissure healing. The procedure is quick, typically taking 15 to 30 minutes, and the success rate exceeds 90% for healing chronic fissures. Studies consistently demonstrate that surgery is significantly more effective than any medical treatment for chronic fissures, with long-term relief and low recurrence rates.
However, LIS does carry a small risk of complications, particularly minor fecal incontinence. A small percentage of patients may experience difficulty controlling gas or mild stool leakage following the procedure. These side effects are usually temporary and improve over time as the area heals and the remaining sphincter muscle compensates. The risk of permanent incontinence is very low, estimated at less than 5%, but patients should discuss this potential complication with their surgeon before proceeding with surgery.
Post-Operative Care and Recovery
Following surgical treatment for anal fissures, proper post-operative care is essential for optimal healing and preventing complications. Patients should continue following a high-fiber diet and maintaining adequate hydration to ensure soft, regular bowel movements. Good hygiene practices, including gentle cleansing with pre-moistened wipes and regular sitz baths, help prevent infection and promote comfort during the healing process.
Most patients can resume normal activities within a few days after surgery, though heavy lifting and strenuous physical activities should be avoided for several weeks. Pain medication may be prescribed for the first few days post-operatively, and stool softeners should be continued to prevent constipation. Follow-up appointments with the surgeon allow for monitoring of healing progress and early detection of any complications.
Treatment Duration and Expectations
The timeline for anal fissure healing varies depending on whether the fissure is acute or chronic and which treatment approach is used. Acute fissures often heal within a few weeks with appropriate home treatment, including dietary modifications, adequate hydration, and regular sitz baths. However, patients should understand that healing takes time, and it may take six weeks or longer to achieve complete resolution even with optimal treatment.
All topical treatments for anal fissures should be applied consistently for at least six weeks to allow complete re-epithelialization of the fissure. Discontinuing treatment too early, even if symptoms improve, can result in recurrence. Chronic fissures typically require longer treatment periods and may ultimately need surgical intervention if medical management proves insufficient.
Preventing Anal Fissure Recurrence
Once an anal fissure has healed, prevention of recurrence becomes the primary goal. Many of the same strategies used to treat fissures also serve as preventive measures. Maintaining a high-fiber diet, staying well-hydrated, and establishing regular bowel habits help ensure soft stools that pass easily without causing trauma to the anal canal.
Patients should avoid straining during bowel movements and respond promptly to the urge to defecate rather than delaying, which can lead to harder stools that are more difficult to pass. Some individuals benefit from continuing fiber supplements or stool softeners long-term to maintain optimal stool consistency. Avoiding foods that trigger diarrhea or constipation helps maintain digestive regularity and reduces stress on the anal canal.
Regular physical activity promotes healthy bowel function and can help prevent constipation. Patients should also avoid sitting on the toilet for prolonged periods, as this can increase pressure on the anal area. For individuals prone to anal fissures, these lifestyle modifications become permanent habits that significantly reduce the risk of recurrence.
When to Seek Medical Attention
While many anal fissures can be successfully treated at home with conservative measures, certain situations warrant professional medical evaluation. Patients should consult a healthcare provider if symptoms persist despite several weeks of appropriate home treatment, if pain becomes severe and unmanageable with over-the-counter pain relievers, or if bleeding becomes heavy or persistent.
Additionally, if symptoms suggestive of anal fissure are accompanied by fever, discharge, or signs of infection, immediate medical attention is necessary. Individuals with underlying conditions such as inflammatory bowel disease, HIV, or other immunocompromising conditions should seek medical evaluation promptly rather than relying solely on home treatment. Healthcare professionals can properly diagnose the condition, rule out other serious problems with similar symptoms, and recommend appropriate treatment escalation when conservative measures prove insufficient.
Frequently Asked Questions
Q: How long does it take for an anal fissure to heal completely?
A: Acute anal fissures typically heal within four to six weeks with appropriate conservative treatment including dietary changes, adequate hydration, and regular sitz baths. Chronic fissures may require several months of treatment with topical medications or may ultimately need surgical intervention for complete healing.
Q: Can I use over-the-counter hemorrhoid creams for anal fissure treatment?
A: While some hemorrhoid creams may provide temporary pain relief, they are not specifically designed to treat anal fissures and may contain ingredients like witch hazel that can irritate the sensitive area. It’s better to use treatments specifically recommended for fissures, such as topical nitroglycerin or calcium channel blockers prescribed by a healthcare provider.
Q: Is surgery always necessary for chronic anal fissures?
A: No, surgery is not always necessary. Many chronic fissures respond to topical medications, Botox injections, or a combination of treatments. Surgery is typically reserved for cases that don’t respond to conservative and medical management after adequate treatment duration, usually at least eight weeks.
Q: Will I experience incontinence after lateral internal sphincterotomy?
A: While there is a small risk of minor incontinence following LIS, permanent incontinence is rare, occurring in less than 5% of cases. Most patients who experience any incontinence symptoms find they are temporary and improve as healing progresses. The high success rate of the procedure generally outweighs this small risk for patients with chronic fissures.
Q: Are there foods I should avoid while treating an anal fissure?
A: Yes, it’s advisable to avoid acidic foods such as tomato sauce and citrus fruits, as well as spicy foods that may irritate the area during bowel movements. Also limit foods that cause constipation or diarrhea. Focus instead on high-fiber foods, adequate hydration, and meals that promote regular, soft bowel movements.
Q: Can anal fissures recur after successful treatment?
A: Yes, anal fissures can recur, especially if the underlying causes such as chronic constipation or hard stools are not adequately addressed. Maintaining a high-fiber diet, staying hydrated, avoiding straining during bowel movements, and responding promptly to the urge to defecate are essential preventive measures that reduce recurrence risk.
Q: How often should I take sitz baths for anal fissure treatment?
A: For optimal therapeutic benefit, take sitz baths for 10 to 20 minutes at least two to three times daily, and always after each bowel movement. The warm water helps relax the anal sphincter muscle, reduces pain, improves blood flow, and creates conditions favorable for healing.
References
- https://www.mayoclinic.org/diseases-conditions/anal-fissure/diagnosis-treatment/drc-20351430
- https://www.ncbi.nlm.nih.gov/books/NBK526063/
- https://www.uclahealth.org/medical-services/surgery/colorectal-surgery/patient-resources/patient-instructions/anal-fissure
- https://greaterorlandogi.com/2023/11/22/the-complete-guide-to-anal-fissures/
- https://heritagesurgicalgroup.com/anorectal-surgery/anal-fissure-treatment/
- https://www.ascrsu.com/ascrs/view/ASCRS-Toolkit/2851088/2/Management_of_Anal_Fissures__2023_
- https://bpac.org.nz/BPJ/2013/April/anal-fissures.aspx
- https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=uh3165
- https://www.proctocan.com/a-guide-to-swift-fissure-treatment-and-recovery
Read full bio of Medha Deb